Nasal polyps are benign growths that occur on the mucosal lining of the nasal passages. They are typically small and though noncancerous can still cause obstructions of the sinuses, leading to congestion, breathing problems and sinus infections.
Signs & Symptoms of Nasal Polyps
Some nasal polyps are tiny and cause few problems. Others produce symptoms such as runny nose, congestion, sneezing, loss of smell and taste, postnasal drip, headache, sinus pain and pressure and snoring. If symptoms persist longer than ten days and are not associated with a cold or allergies, seek medical attention. Even though nasal polyps are benign, if left untreated they can grow large enough to cause serious complications including obstructive sleep apnea, meningitis, blood clots and aneurysms.
Causes of Nasal Polyps
Some people develop nasal polyps randomly, but most often there is some sort of triggering mechanism. Common triggers include asthma, hay fever, chronic sinus infections, cystic fibrosis and sensitivity to aspirin and other NSAIDs. Genetics may also play a role.
A diagnosis is usually made through visual inspection with an otoscope or nasal endoscopy. An imaging test, either a CT scan or MRI, can be useful in determining the size of the polyp and in ruling out more serious growths, such as tumors. Allergy tests may be administered in order to identify the substance responsible for your symptoms.
Treatment for Nasal Polyps
Nasal polyps can be treated with either medication or surgery. The goal is to reduce the size of the polyp or remove it completely in order to alleviate your symptoms. Nasal sprays, oral or injectable steroids, antihistamines and antibiotics are all common drug treatments. If they are ineffective, surgery may be performed. The type of procedure depends on the size of the polyp.
An outpatient procedure called a polypectomy uses a suction device or microdebrider to remove the lesion and surrounding tissue, and is effective for treating smaller polyps. Larger ones may require endoscopic sinus surgery. In this procedure, a camera is mounted on a flexible tube, and tools on the end are used for excising the polyp.
SINUVA
ENT Center Of The Ozarks offers a non-surgical procedure for patients who suffer from repeat nasal polyps with SINUVA™ (mometasone furoate) Sinus Implant. SINUVA is proven to reduce polyps and nasal congestion and obstruction.
What Is SINUVA
SINUVA is a sinus implant that treats nasal polyps without surgery. During a routine office visit, a physician will use topical and/or local anesthesia to numb your nose and sinuses. SINUVA is then placed in the sinus cavity through the nasal opening.
How SINUVA Works
Its innovative design provides a 2-in-1 approach: it is designed to open in the sinus cavity and release anti-inflammatory medicine to treat nasal polyps for up to 90 days.
SINUVA Benefits
At 90 days, patients saw:
- Significantly reduces nasal obstruction and congestion
- Significantly improves impaired sense of smell
The most common adverse reactions observed in a clinical trial were bronchitis, upper respiratory or middle ear infection, headache, light-headedness, asthma and nose bleed. SINUVA is indicated for adults with nasal polyps who have had ethmoid sinus surgery.
Patient Testimonial
If you are suffering from chronic or recurring polyps, contact us at (479) 750-2080 to discuss treatment options.

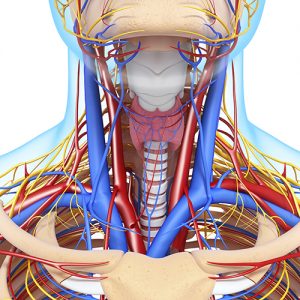 The thyroid and parathyroid are endocrine glands near the throat that secrete hormones throughout the body. The parathyroid is a cluster of smaller glands located near the back of the thyroid that controls the amount of calcium in the blood.
The thyroid and parathyroid are endocrine glands near the throat that secrete hormones throughout the body. The parathyroid is a cluster of smaller glands located near the back of the thyroid that controls the amount of calcium in the blood. 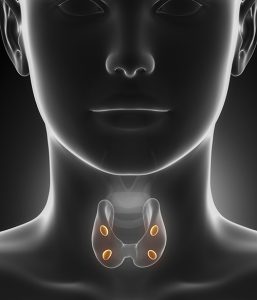 Thyroid nodules are lumps or cysts that form in the thyroid. Many are simply an overgrowth of normal thyroid tissue. These lumps can be buried deep in thyroid tissues or may be located near the edge and feel like a lump in the skin. In some cases, they can even be visible in the front of the neck. Most of the time they are found and identified during routine checkups.
Thyroid nodules are lumps or cysts that form in the thyroid. Many are simply an overgrowth of normal thyroid tissue. These lumps can be buried deep in thyroid tissues or may be located near the edge and feel like a lump in the skin. In some cases, they can even be visible in the front of the neck. Most of the time they are found and identified during routine checkups. 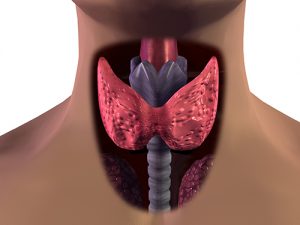 The thyroid and parathyroid are endocrine glands near the throat that secrete hormones throughout the body. The thyroid is bowtie-shaped and rests in front of the trachea (windpipe). It uses iodine from food to regulate the body’s energy. The parathyroid is a cluster of smaller glands located on the back of the thyroid. Their role is to control the amount of calcium in the blood.
The thyroid and parathyroid are endocrine glands near the throat that secrete hormones throughout the body. The thyroid is bowtie-shaped and rests in front of the trachea (windpipe). It uses iodine from food to regulate the body’s energy. The parathyroid is a cluster of smaller glands located on the back of the thyroid. Their role is to control the amount of calcium in the blood.  CPAP
CPAP Symptoms of sleep apnea include chronic snoring, morning headaches, memory and learning problems, irritability, depression, mood swings, waking up frequently, bed wetting, dry mouth, sore throat and sleepiness during the day. Sleep apnea disrupts the natural sleep cycle, which causes many of the above symptoms despite having “slept” most of the night.
Symptoms of sleep apnea include chronic snoring, morning headaches, memory and learning problems, irritability, depression, mood swings, waking up frequently, bed wetting, dry mouth, sore throat and sleepiness during the day. Sleep apnea disrupts the natural sleep cycle, which causes many of the above symptoms despite having “slept” most of the night.