Our voices are essential for communication. Voice can be manipulated to convey emotion, alert someone of danger and create music. The human voice can create sounds and articulations used in thousands of languages across the world. We use our voices every day without even thinking about how they work.
The mechanism that generates the human voice is made up of three major parts: the lungs, the vocal cords and the articulators. The lungs act as the pump that supplies air flow and pressure to vibrate the vocal cords. The vocal cords, part of the larynx, are vibrating valves that dissect airflow into pulses (soundwaves). The larynx adjusts the length and tension of the vocal cords to affect pitch and tone. Articulators (tongue, palate, cheek and lips) filter soundwaves emanating from the larynx and turn them into words.
You may have a voice disorder if you have trouble controlling pitch, volume, tone or other voice qualities. It means there is something wrong with one of the parts listed above. Symptoms of voice disorders include quivering sound, hoarseness, choppiness, breathiness or unusual pitch. Other symptoms are physical, like feeling a lump in your throat when speaking, feeling tired in your throat or voice box and tenderness on the outside of your throat.
Treatment of voice disorders depends on the cause. Lifestyle changes could help with voice strain from yelling or singing regularly. Speech therapy with a speech-language pathologist (SLP) can help certain voice disorders where muscles are affected. Medicine can help voice disorders that are caused by hormone or thyroid problems. Surgery is also a possibility for those with growths on or near the vocal cords or larynx.
 Vocal Cords
Vocal Cords
The vocal cords are two membranes that stretch horizontally across the larynx. They vibrate to create soundwaves. The cords are controlled by the vagus nerve, which opens the membranes for breathing and contracts them during swallowing and for speaking. Men generally have longer and thicker vocal cords than women, which is why they have deeper voices. Children’s vocal cords are much shorter than adults’, which is why their voices are higher but deepen as they grow. Genetic factors can also affect vocal cords and voice.
Hoarseness
Hoarseness is a symptom, not a disease in itself. It can be defined as any deviation from the voice’s normal quality such as raspiness, breathiness or strain. It is commonly caused by dry throat, dehydration, acid reflux, smoking, strain from excessive screaming or singing, allergies and coughs or colds. It can also, along with other side effects, suggest polyps on the vocal cords, throat or lung cancer, or thyroid conditions.
Laryngitis
Laryngitis is inflammation of the voice box due to vocal strain, irritation, inflammation or infection. Symptoms of laryngitis include hoarseness, voice loss, rawness of the throat, sore or dry throat and cough. Acute laryngitis generally heals on its own or with at-home remedies like rest and drinking warm fluids. Chronic laryngitis is defined as symptoms that persist more than two weeks, which could point to a more serious condition. Seek immediate medical attention if you experience fever, trouble swallowing, trouble breathing, coughing up blood and excessive drooling.
Chronic Cough
Chronic cough is defined as a cough that lasts at least eight weeks in adults or at least four weeks in children. This condition can interrupt sleep and cause vomiting, lightheadedness and even rib fractures. The most common causes of chronic cough are tobacco use, postnasal drip, asthma and acid reflux. Treating the underlying condition is the only way to completely eliminate chronic cough.
 Thyroid nodules are lumps or cysts that form in the thyroid. Many are simply an overgrowth of normal thyroid tissue. These lumps can be buried deep in thyroid tissues or may be located near the edge and feel like a lump in the skin. In some cases, they can even be visible in the front of the neck. Most of the time they are found and identified during routine checkups.
Thyroid nodules are lumps or cysts that form in the thyroid. Many are simply an overgrowth of normal thyroid tissue. These lumps can be buried deep in thyroid tissues or may be located near the edge and feel like a lump in the skin. In some cases, they can even be visible in the front of the neck. Most of the time they are found and identified during routine checkups. 
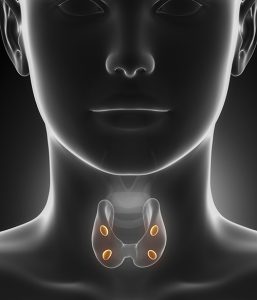
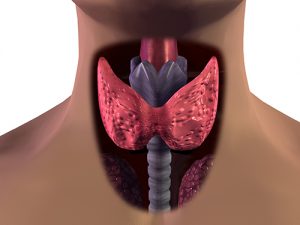 The thyroid and parathyroid are endocrine glands near the throat that secrete hormones throughout the body. The thyroid is bowtie-shaped and rests in front of the trachea (windpipe). It uses iodine from food to regulate the body’s energy. The parathyroid is a cluster of smaller glands located on the back of the thyroid. Their role is to control the amount of calcium in the blood.
The thyroid and parathyroid are endocrine glands near the throat that secrete hormones throughout the body. The thyroid is bowtie-shaped and rests in front of the trachea (windpipe). It uses iodine from food to regulate the body’s energy. The parathyroid is a cluster of smaller glands located on the back of the thyroid. Their role is to control the amount of calcium in the blood.  CPAP
CPAP Symptoms of sleep apnea include chronic snoring, morning headaches, memory and learning problems, irritability, depression, mood swings, waking up frequently, bed wetting, dry mouth, sore throat and sleepiness during the day. Sleep apnea disrupts the natural sleep cycle, which causes many of the above symptoms despite having “slept” most of the night.
Symptoms of sleep apnea include chronic snoring, morning headaches, memory and learning problems, irritability, depression, mood swings, waking up frequently, bed wetting, dry mouth, sore throat and sleepiness during the day. Sleep apnea disrupts the natural sleep cycle, which causes many of the above symptoms despite having “slept” most of the night.  Vocal Cords
Vocal Cords